One of the most common problems of the spine is not -specific pain in the back of the back.According to the National Center for Health Statistics, 26-32% of the adult population suffers from chronic lower back pain.Osteochondrosis is a common cause of such pain.
Osteochondrosis is a premature wear and aging of intervertebral discs and vertebrae.Osteochondrosis can occur in any part of the spine: cervical, thoracic, lumbar or lumbar.The lumbar segment is most often affected and lumbar osteochondrosis develops.If you do not start treating it on time, the disease can affect several departments at a time.
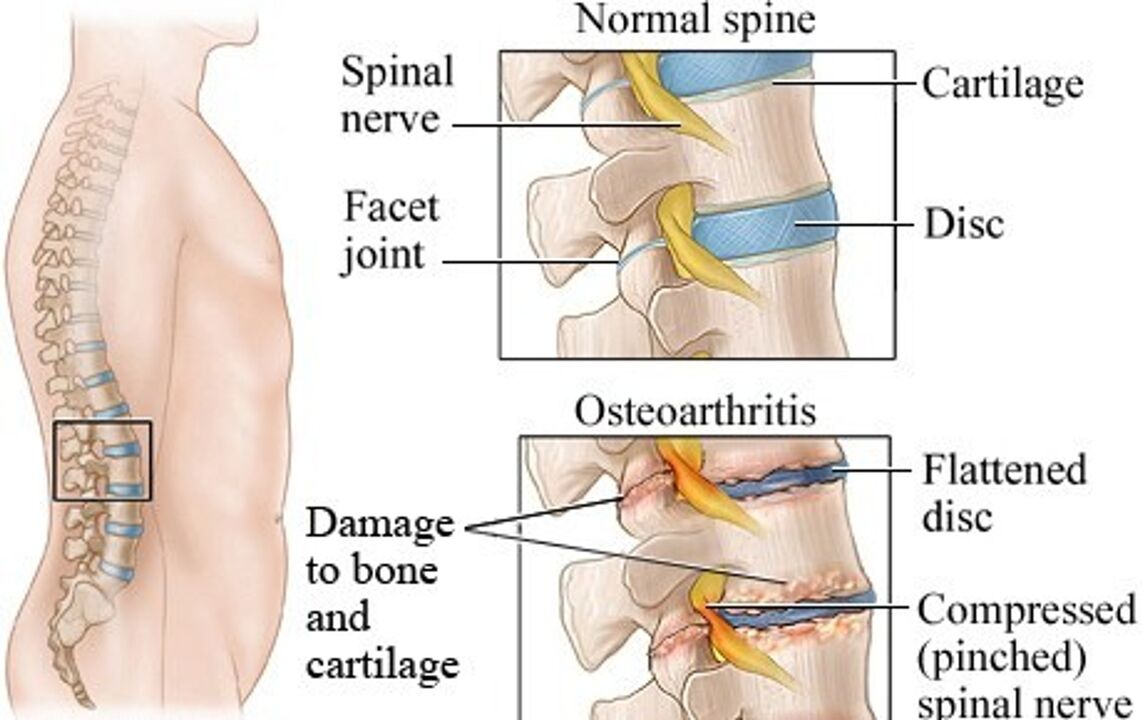
Osteochondrosis of the lumbar region is a chronic degenerative disease in which the cartilage tissue of the intervertebral discs in the lumbar region is destroyed.There are two main parts in the intervertebral disc: the core and the fibrous ring.With increased loading, these structures are destroyed, which leads to compression of the nerves and the appearance of acute pain.
As the disease develops slowly, its signs are difficult to note at the beginning.The patient does not pay attention or even understands exactly where it hurts.Because of this, they often come to the doctor the moment the intervertebral hernia develops.
The causes of osteochondrosis
Lumbar osteochondrosis, like most diseases of the musculoskeletal system, has a non-infectious etiology.The risk factors for the development of osteochondrosis are mainly related to the motor activity of a person, lifestyle, professional working conditions, as well as with heredity.Let's focus on the main and probably the most important factors.
Standing and reduction of motor activitySGiven the modern rhythm of life, people have to be in one position for a long time, whether it is office work, driving a car or training.Therefore, a large number of people have problems with posture disorder, including scoliosis.When the stand is broken, the load on the spine is distributed unevenly: some discs are loaded more than others.The lumbar region suffers more than others.And in the case of the lumbar department, this load is many times more than in other departments.
Excessive physical activitySWhen a person does not exercise and the muscles on his back are weak, intense workouts can harm.Exercises with extra weight and excessive loading of the lumbar region lead to injuries, the intervertebral discs are worn some time ago.
Excess body weight and obesityIncrease the axial load on the spine.At the same time, nutrition of the intervertebral discs is impaired because of the dystrophic processes.
Age -related changesSAfter 60 years, the processes of tissue repair are delayed so that in older people the likelihood of developing intervertebral hernias higher.
Hereditary factorsSIf a person is naturally disturbed by the properties of cartilage and bone tissues, then his osteochondrosis develops early and will be faster.
The first signs and the main symptoms of lumbar osteochondrosis
The intervertebral discs soften the shocks as they walk, run and jump.Due to the structural changes that accompany lumbar osteochondrosis, this function suffers.
When the intervertebral discs for osteochondrosis become slower, this leads to an increase in the vulnerability of the nerves and blood vessels.The nerves are pressed and their nutrition is impaired, acute pain and other symptoms of lumbar osteochondrosis appear.
Acute and chronic lower back pain- This is the main complaint of lumbar osteochondrosis.Personal activity, hypothermia, uncomfortable posture can cause pain.Sometimes the pain extends to the whole back and legs.
Tingling, burning and tingling (paresthesia) in the lower back and legs-A premeditated symptom of lumbar osteochondrosis, which occurs due to nerve compression.
Increasing the tone of the posterior muscles in the lumbar regionThis can increase pain and lead to a decrease in mobility.
Stages of osteochondrosis of lumbar
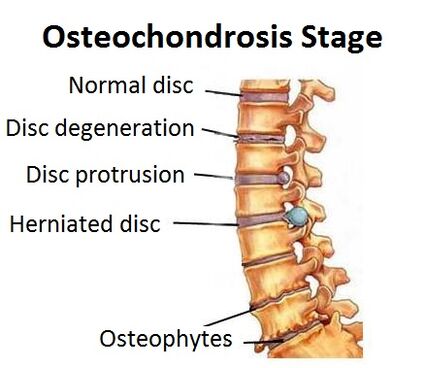
Changes in cartilage and bone tissue appear slowly.Depending on the spread of the pathological process, four stages of lumbar osteochondrosis are distinguished.
1st stageSThis is the onset of the disease (chondrosis).The location of the gelatin nucleus of the disc relative to the fibers of the fibrous ring changes.This leads to nerve irritation and pain.Sometimes nothing hurts at this stage.
Stage 2SDue to the displacement of the discs, the intervertebral gaps are reduced, cracks appear in the discs.The nerves are compressed and the patient suffers from acute lower back pain.
Stage 3SThe intervertebral discs are completely damaged, the fibrous ring is destroyed.At this stage, the risk of developing intervertebral hernia is high.The pain is exacerbated, occurs more frequently and is of a different character: from acute to chronic pain.
Stage 4SThe disease is applied to nearby tissues.In the lumbar region, mobility is reduced, pain occurs even with small changes in the position of the body.At this stage, intervertebral hernias develop and the risk of nerve compression and blood vessels in the lumbar region is high.
Diagnosis of osteochondrosis of lumbar
If you are tormented by acute pain in the lower back, both when moving and at rest, tingling your legs - contact a neurologist.He will check, determine the probable cause of pain and prescribe the necessary diagnosis.
The main methods of examination are radiography and tomography.
- Vision, view and functional radiography of the spine in two projections.This method allows you to evaluate the condition of the spine, but the soft tissues (such as muscles) and cartilage in the photos are not displayed.
- Computer tomography allows you to get more information as the photos are obtained in different projections.Based on the results of the study, the doctor may determine the degree of damage to the lumbar spine.
- Magnetic resonance is the "gold standard" for the exact diagnosis of "lumbar osteochondrosis".According to MRI, the doctor can evaluate the condition of the soft tissues and identify the hernia between the vertebrae.
Treatment of lumbar osteochondrosis
After diagnosing, the neurologist individually chooses treatment.It depends on the stage of the disease and the severity of the symptoms.Most patients are assisted by complete conservative treatment (drug therapy, physiotherapy exercises, physiotherapy).If the patient is no better and serious complications develop, the operation is prescribed.
Conservative treatment
Conservative Treatment Tasks:
- Stop the pain.
- Reducing inflammation.
- Prevention of the development of complications.
- Reduce spinal load by strengthening the muscles of the back.
- Reducing nerve compression.
- In the intervertebral hernia - create conditions for your absorption and natural healing.
In the acute phase of the disease, the doctor mainly reduces pain and inflammation with analgesics and anti -inflammatory drugs.The neurologist then prepares an individual program consisting of physiotherapy, manual therapy and physiotherapy exercises.
PhysiotherapyIt is based on the use of physical factors: cold, heat, electrical current, magnetic radiation, laser and more.They help reduce the intensity of pain and improve tissue nutrition, which contributes to their natural recovery.
KineshitheapIt is active (exercise therapy) and passive (massage, grip).It allows you to strengthen the muscles of the back, relieve muscle tension, improve microcirculation and activate the recovery processes.
Manual therapy and massageRemove increased muscle tone in the lower back, restore mobility.Therefore, the nutrition of the damaged area improves and the degree of pinching of the nerves decreases.
AdhesionOr kinesiological adhesion is based on the use of elastic plasters that are glued to the skin to weaken or enhance muscle tone.Thus, the muscle frame is enhanced, the microcirculation in the lumbar region is improved and the distribution of load on the spine is normalized.
Laser therapyIt is based on the use of low -intensity laser radiation and its positive effects on cell function.It contributes to the natural restoration of the intervertebral discs by improving their diet.
Plasma therapy(PRP therapy)-Methode to improve regeneration processes.Injections of the patient's purified plasma stimulate his immunity.
Reflexology, acupunctureImprove blood supply to the affected areas, reduce pain.
Shock therapy- This is the effect of high frequency waves on the affected area.It stimulates the natural processes of tissue regeneration and improves tissue nutrition.
Orthopedics- Individual choice of corsets for additional support of the spine.Allows partial compensation of the load of the spine.As you wear a corset, the pain decreases, the mobility and quality of life of the patient increase.
Lumbar osteochondrosis is a chronic disease.It is important for the patient to change his lifestyle and learn to live with this disease.For this purpose, there are special educational programs that can improve the quality of life of the patient.
The positive effect of conservative treatment is achieved for 2-3 months.If such treatment is ineffective, the surgery is prescribed.
Work
With the development of intervertebral hernias of the lumbar department, minimally invasive surgery is performed.The choice in the direction of neurosurgical treatment is made with special indications, in severe, threatening the patient's life.
Work is a complex invasive treatment that is related to risks.Complications may develop during or after surgery.And the success of treatment also depends on postoperative rehabilitation, which includes conservative therapy methods and orthopedic correction.
Do not delay the treatment
Lumbar osteochondrosis is a progressive disease.If not detected on time and does not start to cure it, it can lead to damage and reduction of quality of life.Over time, several parts of the spine are affected, the pain made of acute passes into chronic.
Timely prevention of symptoms and treatment of lumbar osteochondrosis in the initial stages can prevent the development of the disease and worsening in the condition.























